A percutaneous coronary intervention, or PCI, is a common procedure performed by a specialist cardiologist to open up arteries that are clogged or narrowed due to fatty deposits.
This procedure is also sometimes referred to as a coronary angioplasty, balloon angioplasty, or stent. A stent is a small mesh tube made of metal, which acts like scaffolding that supports the artery, keeping it open and improving blood flow.
“Percutaneous” simply means “through the skin”, because a catheter is inserted through the skin and into the artery.
A percutaneous coronary intervention is most commonly performed as an elective procedure, but it can also be done as an emergency procedure following a heart attack.
This article explains what happens during a percutaneous coronary intervention (PCI) procedure and the potential risks and complications of the procedure. It also outlines what to expect before, during and after a PCI.
Why is a percutaneous coronary intervention performed?
A percutaneous coronary intervention is a minimally invasive surgical procedure performed by an interventional cardiologist under sedation and local anaesthetic to help restore blood flow to the heart due to blocked arteries.
This will improve the symptoms experienced by patients with partially blocked arteries – such as chest pain (angina) and/or shortness of breath – and help to reduce the risk of a heart attack.
Atherosclerosis is a condition caused by fatty deposits that build up in the arteries leading to the heart. These fatty deposits, or plaque, clog and narrow the coronary arteries and reduce blood flow to the heart. This puts pressure on the heart and it can cause chest pain (angina) or a heart attack (myocardial infarction).
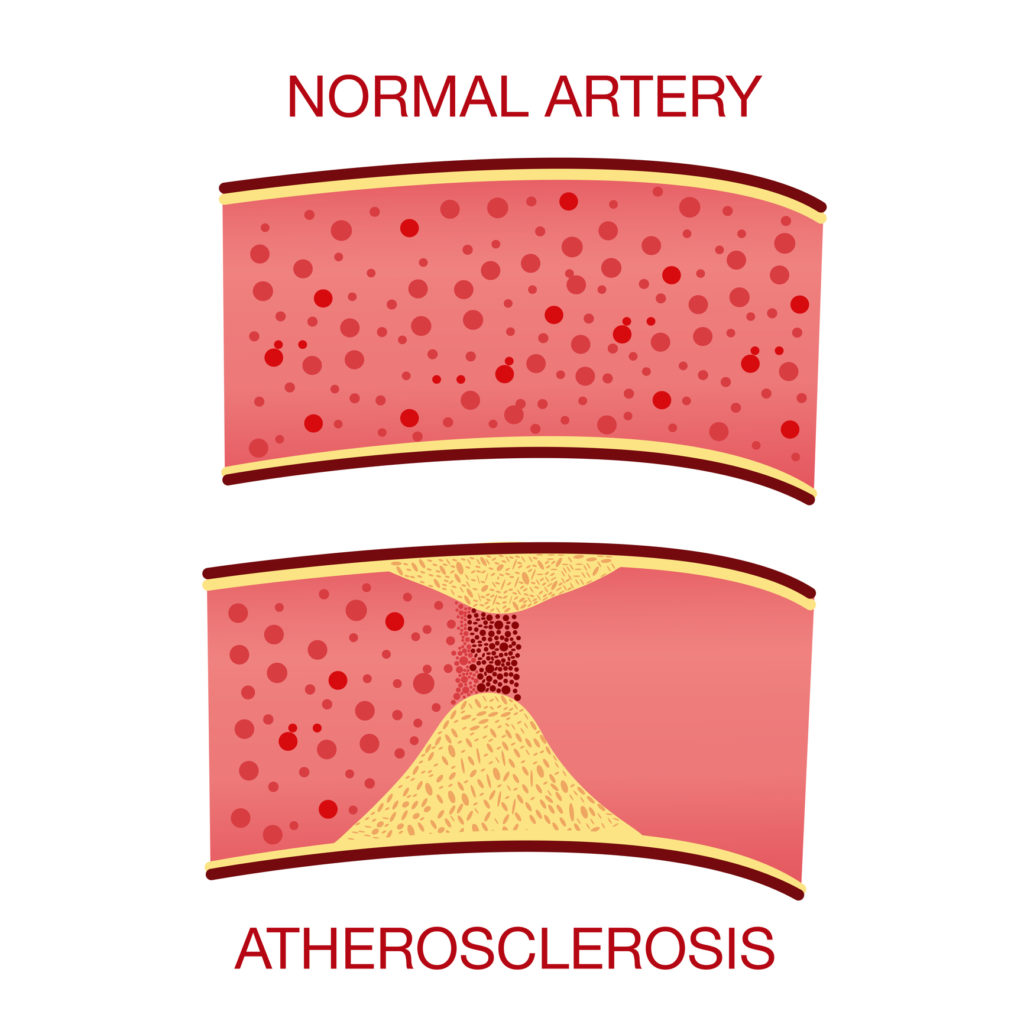
Atherosclerosis is the buildup of fatty deposits in the arteries leading to the heart.
“A PCI will improve blood flow to the heart, helping to prevent angina or a potential heart attack”, says Associate Professor Nigel Jepson, the Medical Director of Eastern Heart Clinic.
“If you’ve had angina or a heart attack, a percutaneous coronary intervention is a life-saving procedure that opens up the arteries. It’s a very common procedure at Eastern Heart Clinic to treat angina or heart attacks to allow the heart to function at its best.”
More than 1,500 PCI procedures have been performed every year at Eastern Heart Clinic since it opened in 2006. Research shows that clinics that perform high numbers of procedures every year have fewer adverse events.
Our highly skilled team of surgeons, anaesthetists and nurses have extensive experience caring for patients undergoing this type of procedure.
Potential risks and complications of a percutaneous coronary intervention
A percutaneous coronary intervention is generally a low risk procedure that’s performed regularly at Eastern Heart Clinic.
However, as with any medical procedure, there is a small risk of complications. You’ll be given information about potential risks and complications by your doctor before your procedure.
It is common to have some bruising and swelling at the site where the catheter is inserted.
While the overall risk of complication is low, more serious risks include:
- an allergic reaction to the X-ray dye
- infection
- bleeding at the insertion site
- pain
- blood clots
- re-narrowing of the artery
- abnormal heart rhythms (arrhythmias)
- heart attack
- coronary artery damage
- stroke
- damage to the kidneys
After the procedure, there is a small risk that blood clots may form within the stent, which can cause a heart attack. That’s why you will need to take blood-thinning medication afterwards to reduce the risk of a clot forming. Your doctor will talk to you about what medication you’ll need to take, and for how long.
If you have any concerns about the procedure, it’s important to discuss these with your doctor before your procedure.
Potential changes to your medications before and after PCI
Some medications may need to be stopped a few days before having a percutaneous coronary intervention, especially if you’re taking medication such as Warfarin, Lasix or insulin.
Your doctor will talk to you about your medications in advance of your procedure. It’s important not to stop or change any medications until you’ve discussed this with your doctor first.
If you’re taking Warfarin, your doctor will tell you whether you need to stop taking it three days before your procedure. You may need to take an alternative anticoagulant (blood thinner) during that time.
“Keep taking your medication until you’ve discussed it with your doctor, who will also tell you if and when to stop taking any medication,” Associate Professor Jepson said.
“Your doctor will let you know when you can start taking your medication again.”
Your doctor will also talk to you about what medication you’ll need to take after a percutaneous coronary intervention. Generally, having a stent means you’ll need to take blood-thinning medication long-term to reduce the risk of developing a blood clot.
If you have any questions about your medication, ask your doctor or phone your cardiology clinic.
How to prepare for a percutaneous coronary intervention
In the weeks leading up to your procedure, you’ll need to have some blood tests and plan your going home arrangements.
On the day of the procedure, you’ll need to start fasting in the morning. At Eastern Heart Clinic, we ask our patients to stop eating solid food six hours before their admission. You can have clear fluids at that time, but no cloudy or milky drinks. Two hours beforehand, you’ll have to stop drinking any fluids, including water.
Your clinic will give you more detailed instructions before admission. You can also read more about fasting before your visit. If you have any questions, contact your clinic beforehand.
What happens during a percutaneous coronary intervention procedure
The percutaneous coronary intervention will be done in a cardiac catheter laboratory, which looks like an operating room. The procedure takes about 90 minutes, depending on the state of your coronary artery or arteries.
Prior to your procedure, you’ll be asked to change into a hospital gown. If you wear glasses and/or hearing aids, most clinics allow you to wear them during your procedure.

Our doctors, nurses and support staff look after you at every stage of the procedure.
You will then be asked to lie down on a narrow procedure table. Your cardiologist, anaesthetist and other experienced cardiology nursing staff will be there to look after you throughout the procedure.
The procedure will be done under either a local or a general anaesthetic. Your surgeon and anaesthetist will talk to you about what type of anaesthetic is best suited to you based on your particular health needs.
Your doctor will let you know where they will insert the catheter. This is generally either the femoral artery in the groin or the brachial artery in the arm. If it’s inserted via your groin, the theatre staff may shave around that area first.
Your anaesthetist will then insert a drip to maintain your fluids, and you’ll be offered sedation to help you relax. You will also be given a local anaesthetic at the site where the catheter (a thin, flexible hollow tube) will be inserted.
A guide wire is then inserted into the artery. An X-ray dye known as “liquid contrast” is injected through the catheter, which can sometimes cause a warm sensation. The dye enables X-ray images of the heart to be taken so your cardiologist can see where the artery has narrowed.
A small balloon catheter is then inserted via the insertion site. This is why percutaneous coronary intervention is sometimes called a “balloon angioplasty”.
The balloon is inflated and deflated several times to open the artery. Then the stent is implanted into the artery, via the catheter. You may feel some discomfort when the balloon is inflated, because the heart will be momentarily deprived of oxygen.
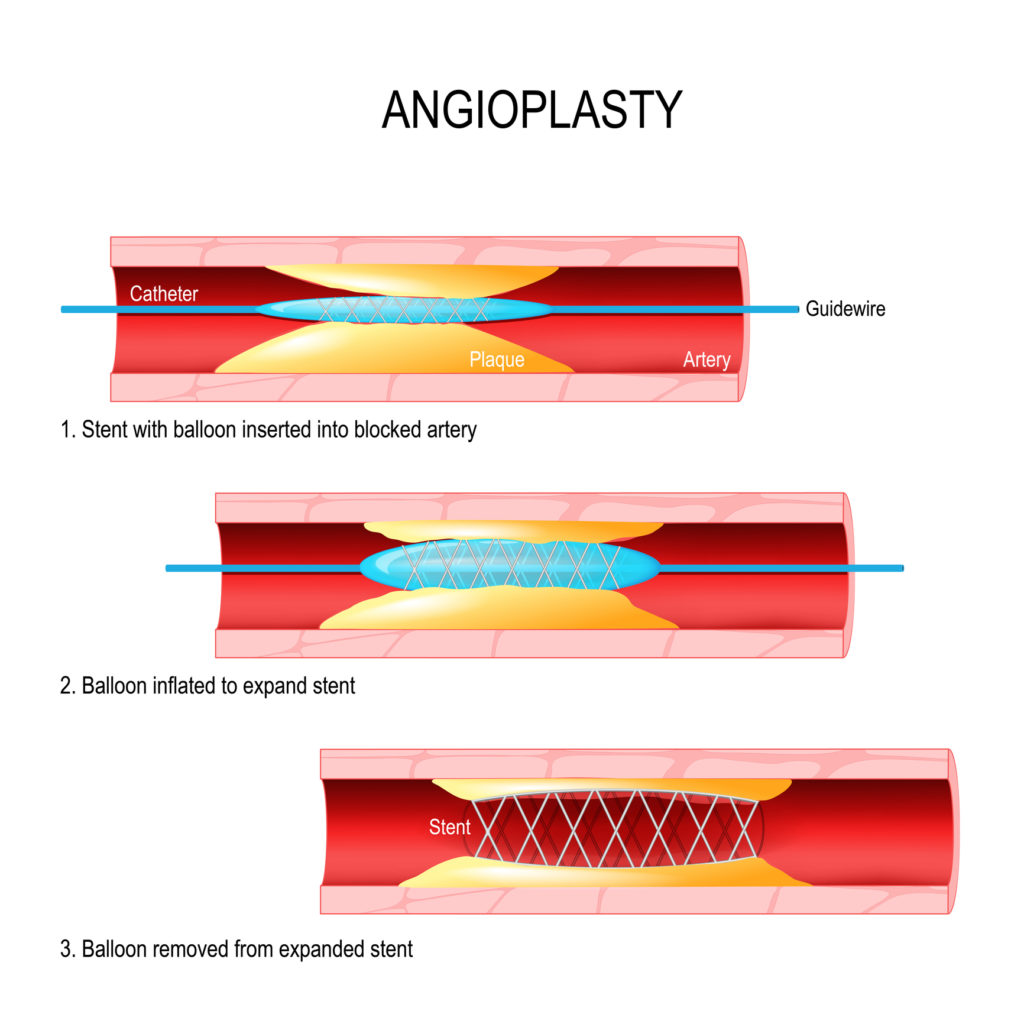
Simple explanation of the inflation of the balloon catheter and insertion of stent.
“Patients sometimes experience angina at this stage of the procedure, but this is only temporary and will resolve as soon as the balloon is deflated,” Associate Professor Jepson says.
“The medical team will be there to take care of you and respond to any pain you may experience.”
The stent is then put into the artery and expanded using the balloon. Unlike the balloon, which is only used during the PCI procedure, the stent remains inside the artery permanently.
Once the stent is in place, the balloon is inflated and the catheter is removed.
What to expect immediately after a percutaneous coronary intervention
After your procedure, you’ll be transferred to the recovery room. You’ll need to lie flat for about four hours and your blood pressure and wound will be closely monitored.
You may experience some discomfort in your chest and, if this is the case, you’ll be offered analgesia to keep you comfortable. You’ll also be encouraged to drink lots of fluids to help flush out the contrast dye.
Sometimes patients stay in hospital overnight following a percutaneous coronary intervention and are discharged home the following morning. This will depend on the time of your procedure, and what your doctor considers is best for you.
Recovering from a percutaneous coronary intervention
As you’ve had sedation for your procedure, it’s a good idea to avoid drinking alcohol or making any major decisions until the effects have completely worn off.
You won’t be able to drive (or fly) for 24 hours afterwards, so you’ll need to arrange for someone to take you home from the hospital. If you live by yourself, we recommend asking someone to stay with you for the first night after the procedure, so someone is close by in case you need any support.
When you’re recovering at home, keep an eye out for any bleeding at the site where the catheter was inserted. It’s normal to have some pain and bruising at the puncture site, but call the clinic if you’re concerned.
Contact your angiogram clinic if you experience any:
- chest pain or tightness
- fever
- swelling or bleeding where the catheter was inserted
- weakness of numbness in the limb where the catheter was inserted
Call an ambulance straight away if you experience:
- significant bleeding or swelling of the wound
- chest pain or tightness that increases or is severe
If you have any general questions or concerns about your recovery, contact your doctor’s rooms or the cardiology clinic for advice.
About Eastern Heart Clinic
Eastern Heart Clinic is an interventional cardiology hospital co-located at the Prince of Wales Hospital at Randwick in Sydney’s eastern suburbs.
One of the largest interventional cardiology hospitals in New South Wales, Eastern Heart Clinic provides diagnostic and interventional cardiology services to public and private patients in metropolitan Sydney and New South Wales.
You can learn more about our clinic, cardiology procedures, and what to expect in advance of your visit.
Read more:
Coronary angiogram: Our complete patient guide
Day of the procedure
Before your visit
After your visit
Patient privacy and rights

Recent Comments