A permanent pacemaker is a small electronic device that helps your heart maintain a regular, healthy rhythm. It’s implanted in your chest to regulate electrical problems with the heart, such as beating too quickly or too slowly.
This guide gives you information about how pacemakers work, what happens during a pacemaker operation and the potential risks and complications.
What is a permanent pacemaker and how does it work?
You may need a pacemaker if you have a heartbeat that’s too slow or too fast, or is irregular. Pacemakers are also commonly used to treat conditions such as congestive heart failure and hypertrophic cardiomyopathy.
Normally, the heart beats when electrical impulses stimulate the heart muscle and make it contract. One part of your heart, called the sino-atrial node, releases electrical pulses which make the heart contract and pump blood to the ventricles, and in turn to the lungs and body.
If your heart has a problem that interferes with those regular electrical impulses, or the “timing” of those electrical impulses is interrupted, you will need a permanent pacemaker.
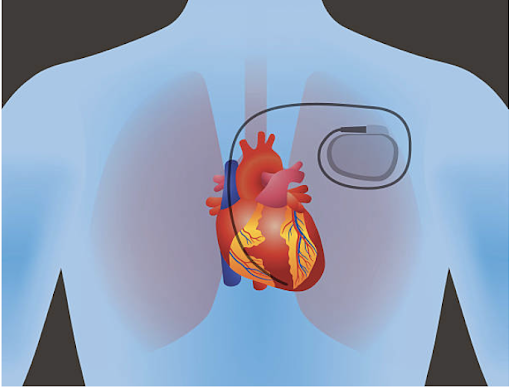
A pacemaker sends regular electrical signals to the heart, helping it pump at a normal, healthy rate. It’s a small battery-powered box that’s implanted into the chest permanently, with small, insulated wires that deliver electrical impulses to your heart. After surgery, the pacemaker sits under the skin near the heart, on either the left or right side of your chest.
Pacemakers are common and will help your heart maintain a healthy heartbeat.
If you’ve had heart problems that have affected your health and lifestyle, a pacemaker will help you be more active. Many patients report feeling more energetic after having a pacemaker.
Are pacemakers all permanent?
There are also temporary or short-term pacemakers, which stay outside your body. Temporary pacemakers are attached to the heart muscle through a small “pacing” wire via a vein or through the chest.
A temporary pacemaker is used to stabilise your heart rate in the short term. This might be needed because of physical trauma, infection, after a heart attack or heart surgery, or while you’re waiting for a permanent pacemaker.
If you have long-term problems with your heart, however, you may need a permanent pacemaker.
What are the signs of needing a pacemaker?
You may need a permanent pacemaker if you have disturbances in your heart’s rhythm. Your heart may beat too quickly or too slowly, or may be irregular (which is known as an arrhythmia).
If you have problems with your heart rhythm, you might have symptoms such as:
- Dizziness
- Fatigue
- Feeling short of breath
- Fainting
If you’re seeing a cardiologist because you have an arrhythmia, you won’t necessarily need a pacemaker. There are different types of arrhythmias, many of which are harmless and don’t need to be regulated with a pacemaker to restore the rhythm.
Your doctor will discuss the best treatment options for you depending on the type of arrhythmia you have.
Are all pacemakers the same?
There are a few different types of pacemakers, and your doctor will decide which one is best for you. Pacemakers have either one, two or three leads, depending on your individual heart problem.
The main types are:
- Single chamber: One lead connecting to one upper or lower chamber of the heart.
- Dual chamber: Two leads connecting to one top and one bottom chamber.
- Biventricular: Three leads connecting to the right atrium, right ventricle and left ventricle. This pacemaker is often used to treat advanced heart failure.
What are the potential risks?
While permanent pacemakers are common, as with any medical procedure there are some potential risks and complications. These include:
- infection at the site of the incision
- swelling, bruising or bleeding
- blood clots near the pacemaker
- blood vessel damage
- collapsed lung
- movement of the leads
Having a pacemaker implanted is generally a safe procedure. However, there are some risks that can occur. Speak to your doctor if you’re concerned.

Our expert team will look after you during every stage of your permanent pacemaker procedure
What happens during pacemaker surgery?
Before surgery, your doctor will discuss what medications you’re taking and whether you need to stop or change anything.
Don’t make any changes to your medications before discussing this with your doctor first. Read more about medication and fasting.
Before your permanent pacemaker procedure, you’ll be attached to a heart monitor and have a drip inserted into your arm. You’ll be given medication to provide pain relief and help you relax.
The surgery will take place in an operating theatre. Once an incision is made near the collarbone, the pacemaker leads are threaded into a large vein on the right side of your heart, and fixed inside the heart using tiny screws.
Your surgeon will program the pacemaker and test it during the procedure. The pacemaker will then be put under the skin, and the incision will be stitched and a dressing applied.
You’ll be at the clinic for about six to eight hours from admission to discharge. The surgery itself takes about one hour. However, you may need to stay at the clinic overnight, and if that’s the case, your doctor will discuss this with you.
What do I need to do afterwards?
After the procedure, you won’t be able to drive for 24 hours, so you’ll need to arrange for someone to take you home afterwards.
You also won’t be able to drive for about two weeks after having a pacemaker implanted.
It’s important to avoid driving because your doctor needs to make sure the leads have had enough time to become fixed in the right position.
About six weeks after the implant surgery, you’ll have a follow-up appointment with your doctor.
Does life change after getting a pacemaker?
Having a pacemaker won’t change your life in any major way, but there are a few things to keep in mind.
Your pacemaker will regulate your heart’s rhythm, but it won’t stop heart disease or plaque building up in your arteries.
It’s still very important to look after your general health: keep up regular physical exercise, eat a healthy diet, avoid smoking and enjoy alcohol in moderation.
Here are some general rules about what you can and can’t do when you’re living with a pacemaker:
- You’ll need to have regular checks, usually once a year. The pacemaker will be checked wirelessly or via Bluetooth, so this won’t be invasive. The battery will also be checked. The pacemaker batteries will last between five and 15 years and your doctor will let you know well in advance when it will need changing.
- It’s a good idea to carry a card in your wallet or bag stating that you have a pacemaker, in case of emergency.
- If you need to have any further surgery, tests or scans, let your healthcare professionals know that you have a pacemaker. MRIs and CT scans can interfere with a pacemaker.
- Avoid putting your mobile phone in a pocket near your chest, and when you’re talking on a mobile hold the phone to the ear on the opposite side to the pacemaker.
- Keep away from electrical generators and high-voltage equipment such as welding equipment.
- Your pacemaker may trigger security alarms at airports, so let security staff know that you have one.
- Tell your doctor if your job involves operating heavy machinery or driving.
- Your pacemaker won’t affect whether you can play sport or have sex. Be wary of any high contact sports, though.
About Eastern Heart Clinic
One of the largest interventional cardiology hospitals in New South Wales, Eastern Heart Clinic provides diagnostic and interventional cardiology services to public and private patients in metropolitan Sydney and New South Wales. It is co-located at the Prince of Wales Hospital at Randwick in Sydney’s eastern suburbs.
Learn more about our clinic, cardiology procedures, and what to expect if you’ll be visiting us for a procedure.
Read more:
What happens during a permanent pacemaker procedure?
Day of the procedure
Before your visit
After your visit
Patient privacy and rights

Recent Comments